Mental health care is changing fast. More people are using apps, wearables, and chatbots to track moods, sleep, and stress, and many of these tools now include automated reporting powered by artificial intelligence (AI). But can a machine really turn scattered data points into meaningful insight about your emotional life? And if so, how reliable are those insights?
This article explains what automated mental-health reporting is, how it works, what the evidence says (with studies and percentages), the real benefits, and the important limitations to watch. I’ve written this to be practical: you’ll get the science, real numbers you can trust, and clear takeaways you can use today.
What is automated mental-health reporting?
Put simply, automated mental-health reporting uses software, often AI and data analytics, to collect, analyse, and summarise information about a person’s mental state. That information can come from:
- Active inputs: mood journals, short surveys (ecological momentary assessments or EMAs), symptom checklists.
- Passive sensors: sleep and activity from wearables, heart-rate variability (HRV), phone usage, and location patterns.
- Conversational data: what you type or say to an AI therapy chatbot (for example, CBT-style interactions).
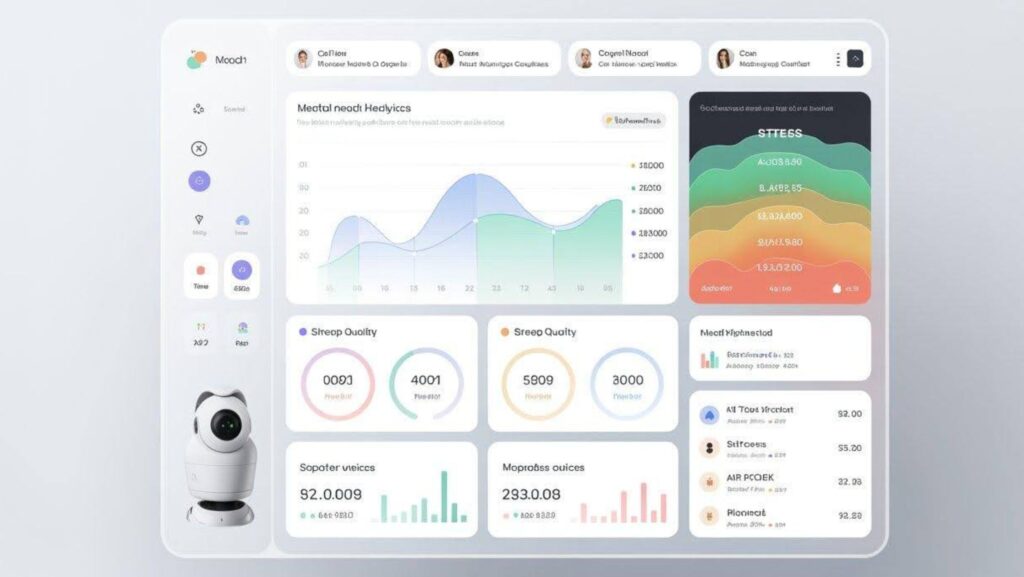
The system then runs analytics to detect trends (for example: “your anxiety tends to be higher on Mondays”), flags anomalies (a sudden dip in mood), and generates human-readable reports (daily summaries, weekly charts, or clinician-facing notes). The idea is to turn noisy, everyday signals into actionable insight.
Why it matters: the case for data-driven mental health
There are three big reasons automated reporting is attractive:
- Scale and continuity. Unlike a weekly therapy session, automated systems can monitor day-to-day changes and provide continuous feedback. This makes it possible to spot shifts before they develop into crises.
- Personalisation. AI can learn which patterns are meaningful for you (not just averages across millions) and tailor suggestions.
- Efficiency for clinicians. Summarised reports let therapists spend more time on interventions and less time collecting history.
Several studies highlight the growing potential of AI therapists in improving mental health outcomes. For instance, clinical trials involving AI-driven conversational agents, often referred to as AI therapists, have shown measurable reductions in symptoms of anxiety and depression.
Likewise, ecological momentary assessment (EMA) research reveals that users consistently engage in short, repeated mood check-ins, providing the continuous data that AI therapist platforms need to deliver accurate and personalised mental health insights.
What the studies say — numbers that matter
Here are the most relevant, evidence-based findings to keep in mind.
1. Chatbots and short-term symptom reductions
Randomised trials of therapeutic chatbots (AI that delivers CBT-style interactions) have shown meaningful short-term improvements. For instance, a recent randomised controlled trial of Woebot found that two weeks of engagement produced significant reductions in anxiety and depressive symptoms, consistent with many chatbot studies reporting 20–30% symptom reductions in short interventions. These are not panaceas, but they do show measurable clinical impact in controlled conditions.
2. EMA compliance rates (people will check in)
Automated reporting relies on people feeding it data. Meta-analytic evidence shows ecological momentary assessment (EMA) — the repeated short surveys many apps use — achieves pooled compliance around 75% (with a typical 95% CI ≈ 72–78%). That’s good: it means a majority of participants respond frequently enough to make automated summaries meaningful.
3. Wearables and physiological signals (HRV, sleep)
Studies linking wearable measures and mental states are promising but mixed. Recent work shows heart-rate variability (HRV) measured via wrist devices correlates with self-reported depression and anxiety symptoms — but effect sizes and reliability vary by device and context. Wearables are most robust for sleep duration and activity; their stress inferences (arousal vs stress) can be noisy. In short: wearables add useful signals, but they’re imperfect and need cautious interpretation.
4. Digital phenotyping & early detection
“Digital phenotyping” — combining passive phone and sensor data with active reports — can help predict mood changes and relapse risk. Reviews indicate potential for early-warning systems, although the accuracy depends heavily on dataset size, diversity, and clinical validation. Some social-media studies (and academic pilots) have shown predictive accuracies in the 60–80% range for specific tasks (for example, flagging depressive language), but results are variable and context-dependent.
5. Privacy red flags
Finally, independent audits warn that many mental-health apps have weak privacy practices: Mozilla’s investigations flagged a large proportion of popular apps for poor data-handling, and policymakers are increasingly scrutinising the space. This makes robust privacy and transparency non-negotiable for any automated reporting system.
Benefits: what automated reports can realistically do for you
When designed and used responsibly, automated mental-health reporting delivers several practical benefits:
1. Reveal hidden patterns
People often don’t see slow trends: missed sleep, creeping isolation, or a link between late-night screen use and low mood. Automated reports quantify these patterns so you can test small changes. For many users, seeing a concrete number or chart is more motivating than vague intuition.
Example: An app might show “On days after <6 hours’ sleep, your self-reported mood falls by ~30% on average”, that’s a clear, testable insight.
2. Timely, personalised nudges
If your HRV drops and you’ve reported higher stress, an AI coach can recommend a 2-minute grounding exercise in the moment. Timely micro-interventions can produce measurable benefits, especially when repeated.
3. Better therapy sessions
Clinicians appreciate concise, data-driven summaries. Weekly automated reports (mood trends, sleep, activity, high-stress days) let therapists skip the “recounting” and focus on what to change. That makes therapy more efficient and may speed up progress.
4. Scaling preventive care
Automated systems can monitor large populations and flag those who may need human follow-up. For healthcare systems and employers, this creates an opportunity for early, low-cost interventions rather than late, high-cost crises.
Limitations and real risks (be honest about them)
Automated reporting is powerful, but not magic. Here are the crucial limitations you should weigh.
1. Signal quality varies
Sensors and self-reports can be noisy. Phone geolocation doesn’t always mean social isolation; a low HRV can indicate excitement instead of stress. Poor signal quality leads to false positives (unnecessary alarms) and false negatives (missed risk).
2. Interpretation is not diagnosis
An automated trend — e.g., “your mood declined 25% this month” — is a signal, not a diagnosis. Clinical assessment requires context, history and human judgement.
3. Privacy and consent are critical
Many mental-health apps have weak privacy safeguards. Automated systems often collect very sensitive data (mood logs, messages, location).

If data are sold or leaked, the harm can be severe. Independent audits (e.g. Mozilla) have flagged this as a pressing concern.
4. Algorithmic bias and equity
If models are trained on non-diverse samples, they can misinterpret behaviour in underrepresented groups. That can worsen disparities rather than reduce them.
5. Over-automation and false reassurance
Relying solely on automated reports risks replacing human contact. AI should augment — not substitute — clinical care, especially for moderate to severe mental-health conditions.
Practical tips: how to get useful automated reporting without the downsides
If you want to experiment with automated mental-health reporting, here’s how to do it safely and usefully.
- Start small. Track one or two reliable signals first (e.g. daily mood rating and sleep hours). Don’t overload the system — quality trumps quantity.
- Choose evidence-backed tools. Prefer apps or services with peer-reviewed research or university partnerships (many chatbots and digital mental-health tools publish studies).
- Read the privacy policy and control sharing. Check encryption practices, data retention policy and whether data are ever sold to third parties. If the policy is vague, treat that as a red flag.
- Use reports as conversations, not diagnoses. Bring weekly summaries to your clinician or a trusted person and use them as starting points for human discussion.
- Watch for alert fatigue. If you get too many warnings, the system is tuned too sensitively. Adjust thresholds to reduce false alarms.
- Keep human escalation rules clear. Any automated system should have easy pathways to human help (hotlines, clinicians) when risk is detected.
Where the field is heading
The near future will likely bring:
- Better multimodal models that combine voice tone, text, movement, and physiology to improve accuracy. Early work in digital phenotyping points to this direction — but clinical validation at scale is still a work in progress.
- Stronger privacy and regulatory standards. Policymakers and watchdogs are increasingly scrutinising mental-health apps; expect a higher bar for transparency and security.
- Hybrid clinical workflows. The most useful systems will integrate automated reporting with human oversight — AI to collect and flag, humans to interpret and treat.
Final takeaways
Automated mental-health reporting is already useful: it can reveal patterns you’d otherwise miss, enable timely nudges, and make therapy sessions more productive. Studies back its promise, chatbot trials show short-term symptom reductions in the 20–30% range, and EMA protocols enjoy pooled compliance of roughly 75%, giving the datasets automated systems need. Wearables add physiological context, though their stress inferences remain imperfect, and digital-phenotyping work shows early promise for detection.
That said, the approach comes with clear caveats: signal noise, privacy risks, algorithmic bias, and the danger of over-reliance. Treat automated reports as insightful prompts, not medical certainties, and always pair them with human expertise when things are serious.
If you or your organisation is considering automated mental-health reporting, aim for evidence, transparency, and clinical integration. Those are the three ingredients that turn raw data into safer, more helpful insight.